Why tiny viruses could be our best bet against antimicrobial resistance
Within a few decades of their discovery, they were largely abandoned in favor of antibiotics. But as antibiotics increasingly fail us, and the deadly threat of antimicrobial resistance looms large, interest in phage therapy is on the rise. We’ve still got a lot to learn about phages, though, and we’ll have to overcome our hatred of viruses before phage therapy becomes mainstream. After all, would you drink a vial of virus?
“There’s an ick factor,” says Chloe James, a microbiologist who studies phages at the University of Salford in the UK.
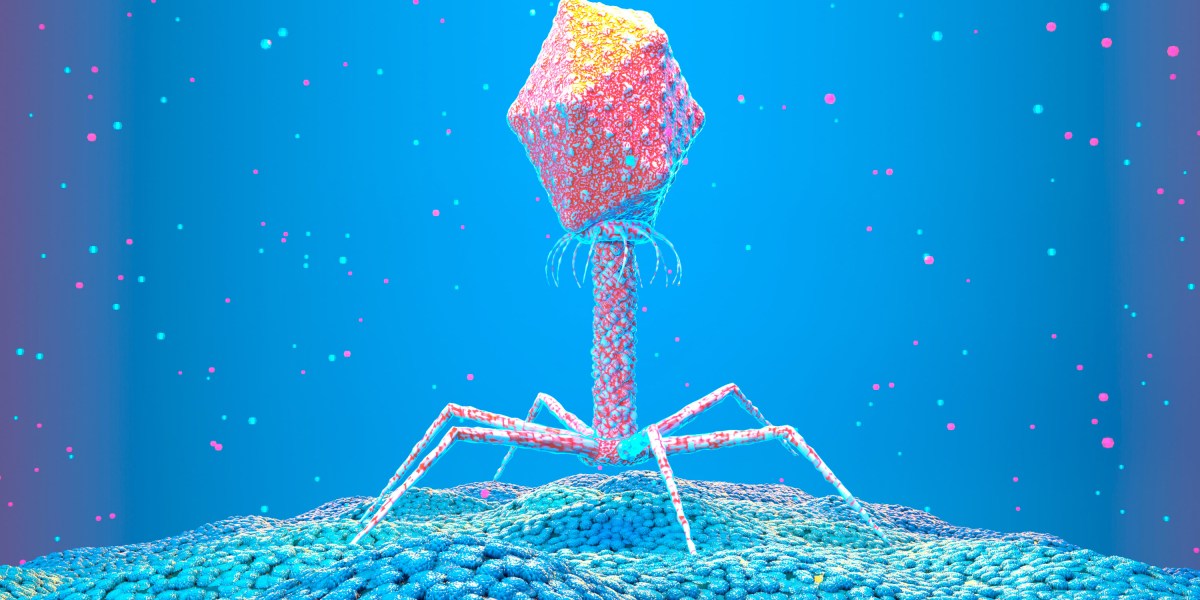
Phages are different from the viruses that infect us, such as the ones that cause flu, Ebola, or covid. Instead, phages specifically infect bacteria. The two have evolved alongside each other—wherever there are bacteria, you’ll find phages infecting them.
In fact, you’ll find phages almost everywhere you look. “They are incredibly diverse, and they’re the most abundant organism on the planet, so they’re literally everywhere,” says James.
Many phages work by landing on a bacterium and injecting their own DNA inside it. There, the DNA can replicate. Eventually, the bacterium itself will burst, emitting an explosion of phages. Not all phages work this way, though. Some insert their genes into the DNA of bacteria. This might stop the bacteria from being able to replicate, or it could give them other powers, such as the ability to cause a more deadly disease or to resist the effects of antibiotics.
It’s complicated, partly because there are so many phages, and partly because they all appear to be incredibly specific. They’ll only infect particular strains of bacteria, for example. But find the right phage for the right bug, and the potential for phage therapy is huge.